
Sometimes this section of your notes will contain only a few snippets of information like, "Patient is sleeping better, no change in the incidence of panic attacks." Some Assessments will be significantly longer than others, based on the complexity of the patient's condition. Like the other sections of SOAP notes, your Assessment should only contain as much information as is necessary. It's essential to reflect on whether your client is showing improvement, maintaining improvements already made, worsening, or demonstrating patterns of remissions. The Assessment will inform your current treatment course as well as future plans, depending on whether the patient is responding to treatment as expected. You will document your impressions and make interpretations based on the information you've gathered.įor an initial visit, the Assessment portion of your notes may or may not include a diagnosis based on the type and severity of symptoms reported and signs observed.įor common conditions such as depression, the Assessment is fairly straightforward and can often lead to a diagnosis in the first visit or two.įor rarer and more complex conditions or those that appear co-morbidly, you may need more time to gather information on the Subjective and Objective levels before arriving at a diagnosis.įor follow-up visits, the Assessment portion of SOAP notes covers an evaluation of how the client is progressing toward established treatment goals. You have a limited window for examination, so it's important to actively look for any signs that complement or contradict information given in the subjective section of the notes.īoth the Subjective and Objective elements previously recorded come into effect in the Assessment phase.
If a client reports having symptoms of anxiety, such as panic attacks, signs of that anxiety might include visible trembling or clenching of muscles as well as hypertension determined by a physical test. Symptoms are the patient's own experience of their condition, whereas signs are objective observations related to symptoms. Record any measurable data during the client's session, including applicable test scores.ĭocumenting the Objective phase brings up the issue of separating symptoms from signs. The Objective phase is concerned only with raw data, not conclusions or diagnoses on your part. What observations can you make about the individual? Write them down as factually as possible. The objective portion of SOAP notes relates to how the body functions and evaluates neurological functioning with the Mental Status Exam. The patient's experience is central to effective treatment, but making observations from an impartial point of view helps round out what the patient told you.
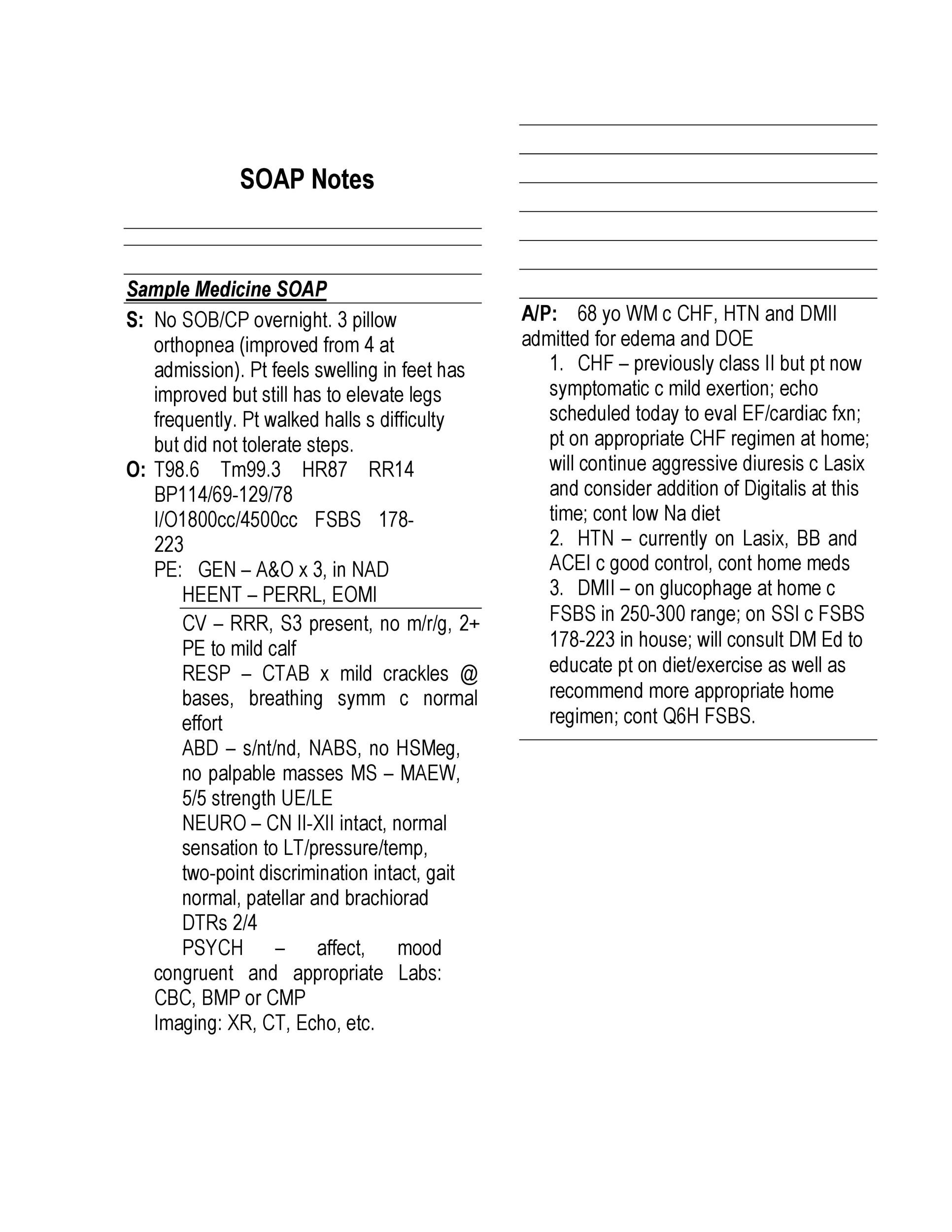
With the client's symptoms fully documented, you can move to the next portion of the note. Symptoms Associated: Are there any secondary symptoms that accompany the patient's main complaint?.Temporal Pattern: Do the symptoms appear in a pattern like in the evenings or after meals?.Radiation: Find out if the pain radiates to other locations in the body.Alleviating or Aggravating Factors: What actions or interactions reduce or increase the severity of the patient's symptoms?.

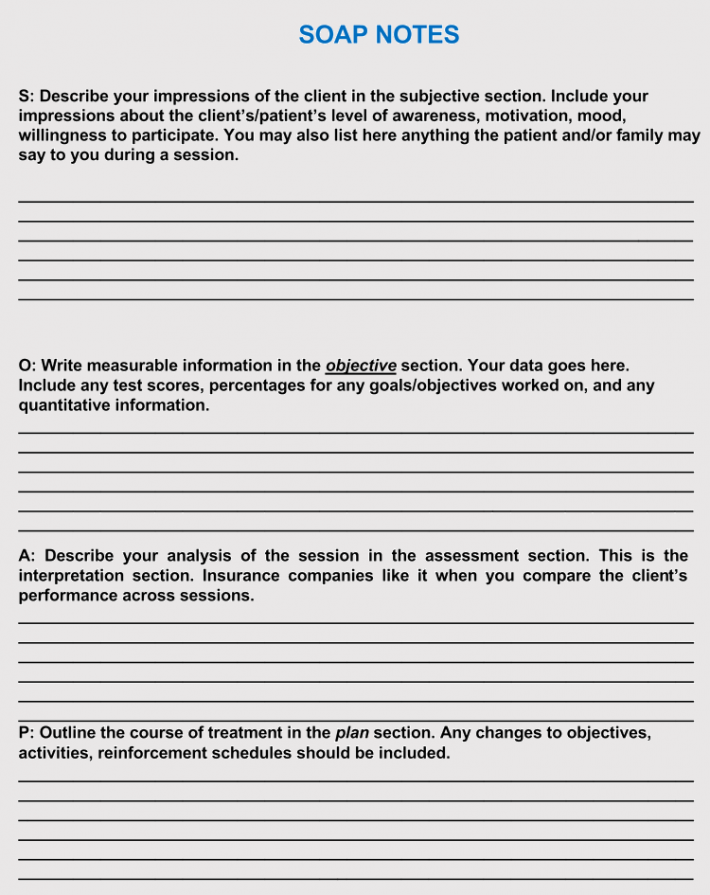
CHaracter: Examine the types of pain - aching, stabbing, etc.Duration: Learn how long the patient has dealt with their symptoms.Location: Find out the primary location of pain or discomfort.Onset: Determine when each symptom first started.The OLD CHARTS acronym provides a smart way to cover a patient's condition systematically: This category is the basis for the rest of your notes as well as your treatment plan, so getting the most quality information possible is paramount. The Subjective category is also an appropriate place to list any comments made by the patient, their family members, or their caretakers. It's crucial to record the patient's own words rather than paraphrasing them so you cultivate the most accurate insight into their condition. The patient will tell you about their experience with the symptoms and condition, as well as what they perceive to be their needs and goals for treatment. The first step is to gather all the information that the client has to share about their own symptoms.


 0 kommentar(er)
0 kommentar(er)
